Myths And Misconceptions

*** Disclaimer: The following article includes information derived from our clinical team’s impressions as specialized professionals working directly with Eating Disorders in Windsor/Essex County.
Common Myths about Eating Disorders
Eating disorders are complex and challenging mental health diagnoses often surrounded by stigma, myths, and misconceptions. It is important to understand the truth about eating disorders and how it affects those in our community. We have addressed some of the most common myths and misconceptions below.
“I know lots of people with an eating disorder, its not that big of a deal”
People with eating disorders experience impairment in their everyday life, and often struggle with anxiety, depression and other mental health challenges in addition to the medical and physical ones associated with the disorder. Research shows that those with eating disorders have the highest mortality rate of any psychiatric illness. Up to 20% of individuals with chronic anorexia nervosa will die as a result of their illness.
Some of the possible medical side effects of an eating disorder:
- Malnutrition
- Low weight/ Obesity
- Growth Delays
- Menstrual Irregularity and Fertility issues
- Increase risk of suicide and self harm behaviours
- Gastrointestinal issues
- Immune deficiency
- Cardia arrythmias
- Skeletal myopathies and Osteoporosis
- Refeeding syndrome
- Rectal prolapse
- Cerebral atrophy
- Cognitive problems
- And many more…
All people with eating disorders are extremely thin or underweight
While there are some people with eating disorders who are underweight, people of all body shapes, sizes and weights can struggle with eating disorders. A person’s weight does not determine their diagnosis, the severity of their disorder (except in the case of Anorexia Nervosa, where BMI dictates severity) or their overall health.
This myth represents the common misconception that Anorexia Nervosa is the only “serious” ED diagnosis; however, Bulimia and other diagnoses have similar mortality rates. Individuals who abuse laxatives or diuretics, or engage in self-induced vomiting are at significantly higher risk of sudden death due to electrolyte imbalances. Chronic excessive exercise also can increase the risk of death in individuals with eating disorders by increasing the amount of stress on the body.
Eating disorders only affect teenagers
People of every age, race and cultural background can develop an Eating Disorder. Pop culture often portrays Eating Disorders as something that teenagers or people in their 20’s struggle with; however, our intake department sees individuals of all ages, including children and the elderly. Within our community, BANA works exclusively with the adult population, the Teen Health Centre (WeCHC) works with adolescents, and the Regional Children’s Centre (WRH) works with children. No matter what age, any individual with eating disorder concerns can contact our general intake number, where they will be connected with appropriate services.
Men don’t get eating disorders
People of all genders struggle with Eating Disorders. Historically, there has been a lot of stigma and shame around men’s mental health, which has contributed to the belief that men are not at risk for developing an eating disorder. However, a 2007 study by the Centers for Disease Control and Prevention found that up to one-third of all those suffering with an eating disorder sufferer are male. BANA and our community partners work with folks of all gender identities, as eating disorders do not discriminate.
The face of ED in Windsor – Essex and the Surrounding Areas
- The average age of BANA’s service recipients is 34.86 years
- Approximately 68% of our client’s self-report additional mental health diagnoses such as depression, anxiety, OCD, bi-polar, PTSD and substance use disorders
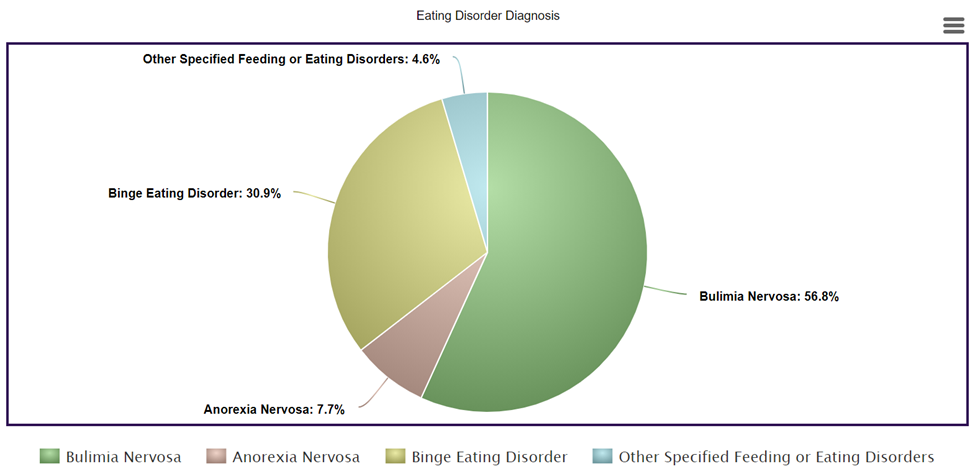
- Our clients are most often diagnosed with Bulimia Nervosa (56.7%), followed by Binge Eating Disorder (30.8%), then Anorexia Nervosa (7.7%); and lastly, Other Specified Feeding or Eating Disorders (4.6%)
Stats come from BANA’s AGM Report 2018-2019
RESOURCES:
https://nedic.ca/eating-disorders-treatment/
https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596
In partnership with Windsor Essex Community Health Centre – Teen Health, BANA provides centralized intake for new client inquiries for residents of Windsor and Essex County.
Intake services are provided to all ages, free of charge and will streamline your access to treatment and provide a continuum of care while answering your questions and requests for assistance.
You can contact the Centralized Intake Worker at 1-855-969-5530 or by completing an inquiry form below.